Severinghaus Lecture underscores brain health in anesthesiology research
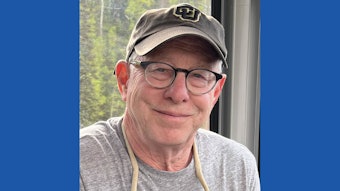
Deborah J. Culley, MD, brain health pioneer to address postoperative neurocognitive disorders.

The 2023 John W. Severinghaus Lecture on Translational Science addressed one of the most debated concepts in anesthesiology research – the effects of anesthesia on cognition and brain function. And the 2024 Severinghaus Lecturer is one of the world’s foremost authorities on how surgery and anesthesia affect the elderly brain.
Deborah J. Culley, MD, has made seminal contributions in this area, as her team was the first to show in animals that an uncomplicated general anesthetic without surgery causes long-lasting learning impairment in the old but not the young. Her lecture, “Perioperative Neurocognitive Disorders: Bench to Bedside,” explored postoperative neurocognitive disorders and trace the transformative events in the field, from Dr. Severinghaus’ early developments in blood oxygen and carbon dioxide measurement, to what we know now about postoperative neurocognitive disorders.
Dr. Culley is the Robert Dunning Dripps Professor in Anesthesia and Chair of the Department of Anesthesiology and Critical Care at the Perelman School of Medicine, University of Pennsylvania in Philadelphia. She is a founding member of the Anesthesia Research Council, a former Director of the American Board of Anesthesiology, former member of the Anesthesiology RRC, and former President of the Society for Neuroscience in Anesthesiology and Critical Care.
After helping to establish that anesthesia and surgery can produce durable changes in cognition and brain function, her research then sought to understand why only some older patients develop postoperative delirium/cognitive dysfunction, while others do not. One potential vulnerability factor she explored was the state of preoperative cognition, which was not normally evaluated in preoperative assessment. Dr. Culley led a series of studies examining the prevalence of cognitive impairment in older surgical patients and its impact on outcomes. This research demonstrated that cognitive screening is feasible in a busy preoperative clinic, revealing a 20%-30% prevalence of impairment in older patients scheduled for elective nonneurological, noncardiac surgery, and confirmed that poor preoperative cognition predicts a higher risk for postoperative delirium and poor outcomes.
Dr. Culley’s work has spurred important changes in clinical practice and stimulated a movement to routinely cognitively screen all older surgical patients preoperatively – a practice now standard at some institutions and recommended in a number of guidelines for the care of older surgical patients.