COVID experiences from the first wave
First wave brought emotional toll, then new knowledge for anesthesiology community.
The learning curve from the first wave of the COVID-19 pandemic was steep and emotional for frontline health care workers. However, the anesthesiology community has worked hard to chart what worked and what didn’t.
The 2021 virtual session “COVID-19 Experiences From the First Wave” painted a stark picture of the pandemic’s impact on health care workers, patients, and their families. It also provided some reassuring protocols for the future, according to Mark E. Nunnally, MD, FCCM, a Professor of Anesthesiology at NYU School of Medicine and a speaker at Friday’s session.
“NYU has a long history of dealing with and adapting to disasters when you consider 9/11 and Hurricane Sandy,” Dr. Nunnally said. “An important part of future planning is logistics. Think about who will care for patients, where they will do it, and what they will do it with. The goal is to have a playbook for a pandemic wave with triggers for contingencies and a step-wise approach to escalating numbers.”
Ironically, several months before the pandemic, NYU Langone Health had an executive simulation for a major viral outbreak. The exercise focused on planning and paid dividends when COVID-19 emerged, he said. The hospital has since repeated the exercise after its real-life experience to build on lessons learned and sharpen its focus in the event of another surge or outbreak.
In looking back at that first wave, Dr. Nunnally said the immediate needs of managing a surge of patients during a respiratory illness outbreak boiled down to prepping facilities and people to care for the patients and providing material to let them do their jobs. Next, he said, came “sustaining the care model, which includes rotating staff and giving them support, along with managing emergent supply issues.” Underlying these principles is a flexible and global approach to operations that accounts for the dynamic nature of the crisis.
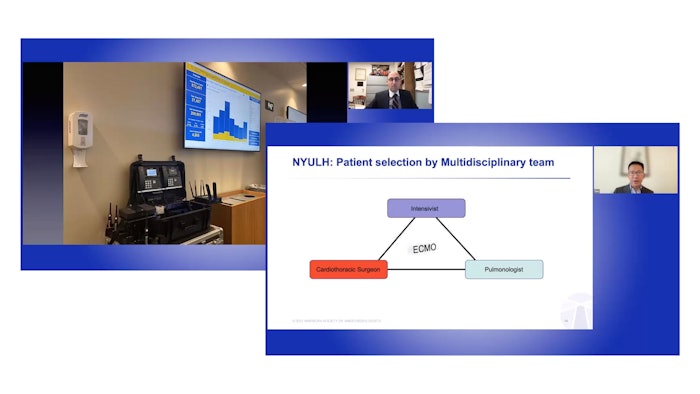
Part of the evaluation from those early days includes the use of extra corporeal membrane oxygenation (ECMO). The most serious patient cases involving COVID-19 require specialized care, including ECMO and early tracheotomy. Fellow panelist Thomas Jan, MD, MPH of NYU Langone Health said that using ECMO benefits patients, but that hospitals must have the facilities, staff, and expertise to use this tool.
“First, you need to know how crippling COVID-19 can be to a hospital system,” Dr. Jan said. “It’s not recommended for every hospital. You have to have the right, skilled personnel, adequate equipment, an equipment supply chain, the rooms, the PPE, protocols, and guides in place as well as the ability to handle the ethical considerations of deciding which patient will get it and which one will not. It’s not easy.”
Dr. Nunnally agreed, and emphasized that in a true pandemic, hospitals will only be able to offer ECMO to a minority of patients.
“Think a lot about triage. Choosing well is important because ECMO COVID-19 patients tend to require a lot of resources for a long time. Encourage your team to be obsessed with finding the flaws in the way they select and manage patients. Everyone has to look for potential sources of failures before they happen,” Dr. Nunnally said. “If you have good experts, they will naturally do this part.”
To break a cycle of mechanical lung injury superimposed on viral injury, Dr. Nunnally said patients on ECMO should be managed to minimize ventilator trauma, including low tidal volumes and modestly high PEEP. Additionally, he suggested the use of the circuit for the gas exchange.
“Teams have to be obsessed with possible failures, so there should be constant vigilance for perfusion, mechanical, coagulation and infectious complications, among many others,” Dr. Nunnally said.
Despite the emotional toll the first wave of the pandemic took on anesthesiologists and other health care providers, Dr. Jan concluded his session with a story about a patient who received ECMO and successfully recovered from the virus.
“There’s a story of Dave Paris who was on America’s Got Talent. We have a video of Dave dancing with a nurse,” Dr. Jan said. “It’s heartwarming to see these patients get better and return to a normal lifestyle.”
Visit Anesthesiology Today Annual Meeting Edition for more articles.









![Sharks[2]](https://img.ascendmedia.com/files/base/ascend/hh/image/2021/10/Sharks_2_.616369899ebe1.png?auto=format%2Ccompress&bg=fff&fill-color=fff&fit=fill&h=191&q=70&w=340)