Treating more than a hip fracture
Greater communication and collaboration are keys to caring for the surgical needs of elderly persons with dementia.
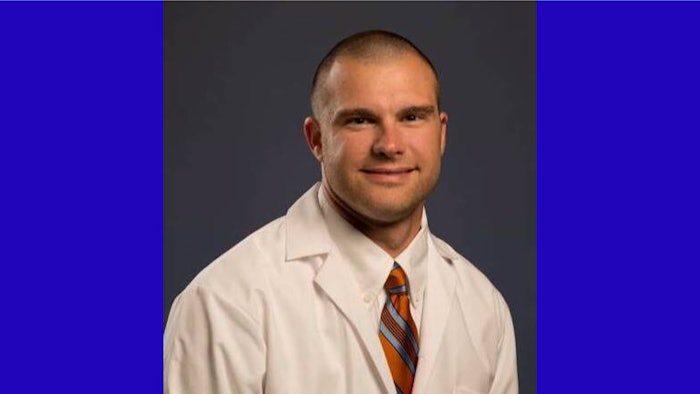
For Paul D. Piennette, MD, MS, the issue of caring for an elderly person with dementia and a hip fracture was personal. Dr. Piennette is an Assistant Professor of Anesthesiology and Perioperative Medicine at the University of Alabama in Birmingham, and the presenter in the 2024 session, “The Elderly Nursing Home Patient With Dementia Has a Hip Fracture: What Are the Anesthetic Considerations?”
As part of the ANESTHESIOLOGY 2024 Geriatric Anesthesia track, this hot topic tackles multiple concerns in the quest to improve patient care outcomes for this population. One of the cases Dr. Piennette discussed involves a member of his own family.
“I was on the other side of the conversation as a patient advocate as opposed to my normal clinical duty that I am more comfortable with, which is why it got me thinking about the complexity of such a case and how a conversation about something like this can be so helpful,” he said.
According to Dr. Piennette, there are several challenges for treating this population. In general, patients with dementia have difficulty with the ability to make informed decisions and to be intimately involved in their own care. Because of this, providers must rely more on family and patient advocates instead of the patients themselves, he said.
Another difficult aspect with this population is communication. Simple questions like “are you in pain?” can become challenging, and when the patient does not feel heard for whatever reason, care becomes more difficult. When packaging all of that alongside the “normal” comorbidities of an aging patient, the best anesthetic plan for a surgery can become quite complex – underscoring the need for these important discussions.
“In my personal experience, the best clinical tip I can give is to draw attention to how important communication and expectations are. When a patient feels they have been heard, their concerns have been considered, and they have a voice in their own care, it makes all the difference in the world,” Dr. Piennette said. “Patients are people, and they know that things happen that are out of their control and things can happen that are sometimes out of the physician’s control. Setting up appropriate expectations with a patient and their family can hedge off very difficult conversations down the road.”
Ultimately, Dr. Piennette said his session was designed to reshape the anesthesiologist's thinking for this population.
“There is not a ‘right’ way to attack some of the problems that we are discussing. Like in life, in medicine, and specifically in anesthesia, there are usually several different ways to get the job done,” he said. “The physician might have a way that they like, the patient or patient’s family might have a different way that they want, and having a discussion and achieving the expectations and goals that everyone has is doable if everyone understands everyone else.”


